HIPAA and Security: Essential Compliance Guide
Healthcare data breaches cost organizations an average of $10.1 million per incident. As such, understanding HIPAA security requirements is about regulatory compliance and protecting your patients, your reputation, and your financial stability. Whether you're a healthcare provider, business associate, or compliance officer, navigating the complex landscape of health information security has never been more critical. This comprehensive guide provides actionable insights to protect sensitive patient information in today's increasingly digital healthcare environment.
To ensure your organization is prepared to handle and prevent data breaches, partner with Tekkis. Our tailored solutions and expert guidance can help you navigate HIPAA compliance and enhance your data security measures. Learn more about how we can support your healthcare organization!
Also Read:

Understanding HIPAA and Its Importance in Health Information Security
The Health Insurance Portability and Accountability Act (HIPAA) represents the cornerstone of health information security in the United States. Enacted in 1996, this federal legislation established comprehensive guidelines that balance accessibility of medical records with robust privacy protections.
Key HIPAA Components
- Privacy Rule: Governs the use and disclosure of Protected Health Information (PHI)
- Security Rule: Focuses specifically on electronic Protected Health Information (ePHI)
- Breach Notification Rule: Requires notification following breaches of unsecured PHI
- Enforcement Rule: Establishes penalties for HIPAA violations
The regulations apply to covered entities (healthcare providers, health plans, and clearinghouses) and their business associates, creating a framework of shared responsibility for protecting health information.
Beyond Compliance: The Business Case for HIPAA Security
HIPAA compliance delivers value beyond regulatory requirements:
- Patient Trust: Demonstrates commitment to protecting sensitive information
- Operational Resilience: Structured security approaches help prevent service disruptions
- Reputation Protection: Avoids damaging public breach notifications
- Financial Security: Prevents costly penalties and remediation expenses
- Improved Data Management: Creates better information governance practices
By implementing comprehensive security measures, healthcare organizations build trust while protecting themselves from increasingly sophisticated cyber threats.
Essential Components of the HIPAA Security Rule
The HIPAA Security Rule establishes national standards to protect individuals' electronic personal health information. Unlike the Privacy Rule, which applies to all forms of PHI, the Security Rule specifically focuses on electronic PHI (ePHI) and provides a framework for ensuring its confidentiality, integrity, and availability.
Security Rule Requirements: Administrative, Physical, and Technical Safeguards
Administrative Safeguards (45 CFR § 164.308)
Administrative safeguards form the backbone of your security program, accounting for over 50% of the Security Rule's requirements:
- Security Management Process: Includes risk analysis, risk management, sanction policy, and information system activity review
- Security Personnel: Requires designation of a security official responsible for policy development and implementation
- Information Access Management: Establishes procedures for authorizing access to ePHI
- Workforce Training: Requires security awareness and training for all staff members
- Contingency Planning: Ensures data backup, disaster recovery, and emergency operations capabilities
- Evaluation: Mandates periodic assessment of security safeguards
Physical Safeguards (45 CFR § 164.310)
These safeguards protect physical infrastructure and devices containing ePHI:
- Facility Access Controls: Limits physical access to facilities while ensuring authorized access
- Workstation Use and Security: Specifies proper functions and physical safeguards for workstations
- Device and Media Controls: Governs receipt and removal of hardware and electronic media containing ePHI
Technical Safeguards (45 CFR § 164.312)
These address technology protecting ePHI:
- Access Control: Implements technical policies for electronic access (unique user identification, emergency access, automatic logoff, encryption)
- Audit Controls: Records and examines activity in systems containing ePHI
- Integrity Controls: Prevents unauthorized alteration or destruction of ePHI
- Transmission Security: Protects ePHI when transmitted over networks
Required vs. Addressable Implementation Specifications
The Security Rule distinguishes between two types of implementation specifications:
Required specifications must be implemented exactly as specified without exception. Examples include:
- Conducting risk analysis
- Appointing a security official
- Establishing contingency plans
- Implementing unique user identification
Addressable specifications allow flexibility based on organizational assessment:
- Assess whether the specification is reasonable for your environment
- Implement if reasonable and appropriate
- If not implementing, document why and implement an equivalent alternative measure
- Document your decision-making process
This distinction recognizes the diverse nature of healthcare organizations while maintaining security standards.
Implementation Challenges by Organization Size
Small Healthcare Practices (1-10 providers)
- Limited Resources: May lack dedicated IT security staff
- Budget Constraints: Need cost-effective security solutions
- Technical Expertise: Often rely on external vendors or consultants
Implementation Strategy: Focus on fundamental controls like strong authentication, encryption, and basic network security. Consider cloud-based solutions with built-in security features.
Mid-sized Organizations (11-50 providers)
- Evolving Infrastructure: Often managing mix of legacy and modern systems
- Growing Complexity: Multiple locations and service lines increase security challenges
- Developing Governance: Transitioning from informal to formal security processes
Implementation Strategy: Establish formal security governance structure, develop comprehensive policies, implement identity management systems, and conduct regular security assessments.
Large Health Systems
- Complex Environment: Extensive network of facilities and technical infrastructure
- Third-party Relationships: Numerous vendors and business associates
- Advanced Threats: Often targeted by sophisticated cybercriminals
Implementation Strategy: Implement enterprise security frameworks, establish security operations centers, deploy advanced threat protection, and develop comprehensive vendor management programs.
Conducting a Comprehensive Risk Analysis
A risk analysis is the fundamental first step in achieving HIPAA compliance. This systematic process identifies vulnerabilities in your systems containing ePHI and evaluates the likelihood and potential impact of threats exploiting those vulnerabilities.
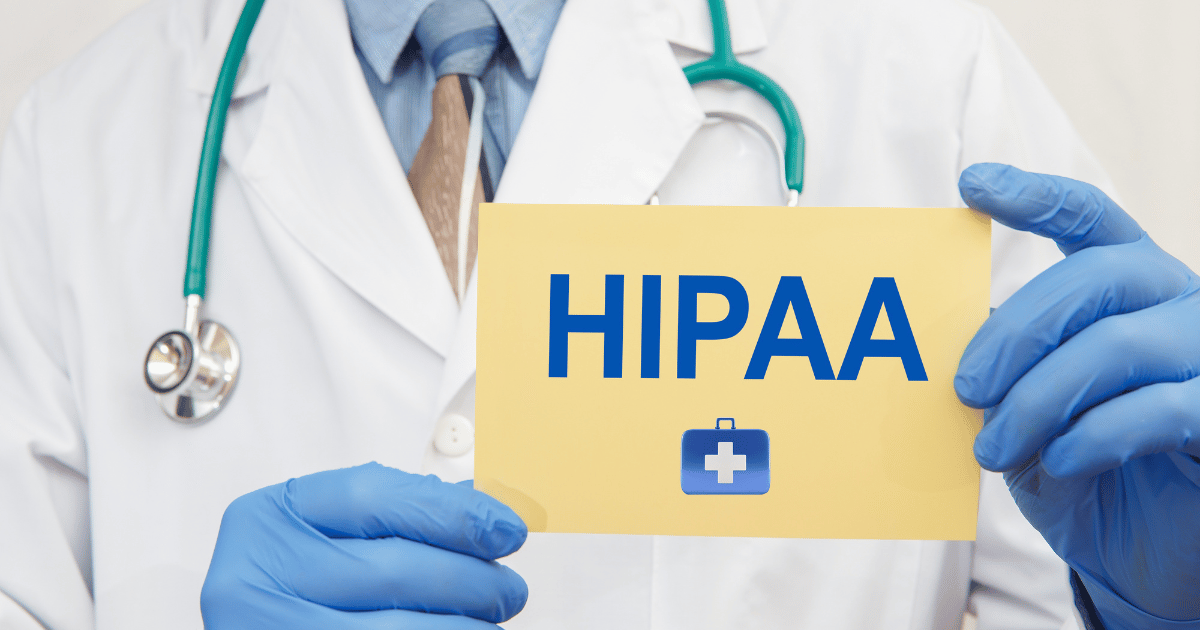
Steps for Effective Risk Assessment and Management
1. Scope the Assessment
- Identify all systems, applications, and devices that create, receive, maintain, or transmit ePHI
- Document data flows across your organization
- Include cloud services, mobile devices, and third-party systems
- Consider both internal and external interfaces
2. Identify Potential Threats and Vulnerabilities
- Technical vulnerabilities (unpatched systems, weak configurations)
- Physical vulnerabilities (facility access, environmental protections)
- Administrative vulnerabilities (inadequate policies, insufficient training)
- Natural threats (fire, flood, power outages)
- Human threats (both malicious actors and unintentional errors)
3. Assess Current Security Measures
- Document existing controls for each system containing ePHI
- Evaluate effectiveness of current security measures
- Identify gaps in protection
4. Determine Likelihood and Impact
- Evaluate probability of threat occurrence
- Assess potential impact if vulnerability is exploited
- Consider business impact, patient safety, and compliance implications
- Use consistent rating methodology (High/Medium/Low or numerical scoring)
5. Determine Risk Level
- Calculate overall risk based on likelihood and impact ratings
- Prioritize risks based on severity
- Document findings in a risk register
6. Develop Risk Management Plan
- Address highest risks first
- Document remediation strategies for each identified risk
- Assign responsibility and establish timelines
- Implement technical, administrative, and physical controls
7. Document and Review Regularly
- Maintain comprehensive documentation of the entire process
- Review and update assessment at least annually
- Reassess after significant changes to systems or operations
Utilizing HHS and NIST HIPAA Security Tools
Several valuable resources can help organizations navigate the complexity of security risk analysis:
- HHS Security Risk Assessment (SRA) Tool: Designed specifically for smaller healthcare providers, this interactive tool walks through each Security Rule requirement while documenting your assessment process.
- NIST Special Publication 800-66: Provides detailed guidance on implementing the HIPAA Security Rule, mapping requirements to specific security controls.
- NIST Special Publication 800-30: Offers a comprehensive risk assessment methodology that aligns with HIPAA requirements.
- NIST Cybersecurity Framework: Provides a structured approach across five core functions (Identify, Protect, Detect, Respond, Recover) that complements HIPAA compliance efforts.
Risk Assessment Checklist
Before completing your risk assessment, verify that you have:
- Documented all systems containing ePHI
- Mapped data flows throughout your organization
- Identified threats to each system component
- Assessed current security measures
- Evaluated likelihood and impact of threats
- Prioritized risks based on severity
- Developed remediation plans for identified risks
- Established timelines for implementing security measures
- Created documentation of the entire assessment process
- Scheduled regular review and updates to the assessment
Technology Selection and Management
Selecting appropriate technology solutions is critical for maintaining HIPAA compliance:
Evaluation Criteria for HIPAA-Compliant Solutions
- Built-in security controls aligned with HIPAA requirements
- Authentication and access control capabilities
- Encryption implementation (both at rest and in transit)
- Audit logging and monitoring features
- Backup and recovery mechanisms
- Vendor security practices and compliance history
- Clear Business Associate Agreement terms
Key Technology Controls
- Identity and Access Management: Single sign-on, multi-factor authentication, role-based access
- Endpoint Protection: Anti-malware, device encryption, mobile device management
- Network Security: Firewalls, intrusion detection/prevention, network segmentation
- Email Security: Encryption, data loss prevention, phishing protection
- Audit Tools: Log management, security information and event management (SIEM)
- Backup Solutions: Encrypted, tested recovery capabilities
HIPAA Compliance for Different Entity Types
Different entity types face unique challenges in implementing HIPAA security requirements.
Covered Entities: Healthcare Providers
Healthcare providers ranging from individual practitioners to large hospital systems must balance security with clinical workflow efficiency:
Implementation Focus Areas
- Clinical System Security: EHR access controls, authentication, audit trails
- Mobile Device Management: Policies for provider-owned and personal devices
- Physical Safeguards: Protecting workstations in high-traffic clinical environments
- Training: Educating clinical staff on security practices that don't impede patient care
Operational Considerations
- Implement single sign-on to reduce authentication burden
- Develop timeout policies appropriate for clinical settings
- Create secure texting solutions for provider communication
- Establish clear protocols for remote/home access to clinical systems
Covered Entities: Health Plans
Health plans manage large volumes of PHI across broad networks of providers and members:
Implementation Focus Areas
- Data Warehouse Security: Protecting large repositories of claims and member information
- Portal Security: Securing provider and member online access points
- Analytics Safeguards: Protecting ePHI used in utilization and quality analytics
- Third-party Integration: Managing connections with numerous external entities
Operational Considerations
- Implement robust identity verification for member portals
- Develop data minimization strategies for analytical environments
- Create comprehensive business associate management programs
- Establish clear data retention and destruction policies
Business Associates: Technology Vendors and Service Providers
Organizations providing services to covered entities have specific compliance obligations:
Implementation Focus Areas
- Contractual Compliance: Meeting security requirements in Business Associate Agreements
- Access Controls: Limiting staff access to customer PHI
- Multi-tenancy Security: Protecting data from multiple covered entities
- Development Security: Implementing secure coding practices
Operational Considerations
- Develop clear documentation of security controls for customers
- Implement customer-specific access restrictions
- Establish comprehensive subcontractor management
- Create transparency around security practices and incidents
Conclusion
Navigating HIPAA compliance in today's rapidly evolving healthcare technology landscape requires vigilance, commitment, and adaptability. Establishing robust security practices is fundamentally about protecting patient trust while enabling efficient healthcare operations.
By implementing the comprehensive framework of administrative, physical, and technical safeguards outlined in the Security Rule, healthcare organizations create multi-layered protection for sensitive health information. Risk analysis serves as the cornerstone of effective implementation, providing insights needed to allocate security resources where they'll have the greatest impact.
Remember that HIPAA compliance is not a destination but an ongoing journey that requires continuous attention. By developing comprehensive policies, implementing appropriate technical solutions, and fostering a culture of security awareness through regular training, healthcare organizations can confidently protect sensitive patient information while delivering high-quality care.
FAQs from Matt from Tekkis
Here are the responses to your questions:
Not at all. The server you’ve purchased is designed to support daily operations across both of your locations—handling workstation management, printer connectivity, network infrastructure, user authentication, cybersecurity protection, and auditing. These functions are all critical to maintaining HIPAA compliance.
While the server can also be configured to host your Dentrix Enterprise practice management software, we would need to assess RAM requirements and potentially add more. RAM is one of the most affordable and easily upgradable components.
This configuration was designed with flexibility in mind, taking into account the uncertainty around whether your practice management application will be hosted in the cloud or in-house. It's important to understand that the practice management software—Dentrix or otherwise—is just one component of your overall technology environment. Onsite devices like workstations, scanners, and printers still require a solid infrastructure, which is best supported by a dedicated server.
No, my recommendation remains unchanged. Currently, about one-third of the dental offices we support use cloud-based practice management applications (such as PracticeWorks Cloud, Curve, or Dentrix Ascend). However, every one of them still relies on an on-premise server to manage local hardware, ensure network performance, and maintain compliance.
No, I would still recommend the same server. It was selected to address the day-to-day technical issues you're currently facing and to improve overall network reliability. The configuration is based on your operational needs, not just the requirements for hosting practice management software.
Additional Note:
A common misconception with cloud-based practice management software is the way it's presented—often referred to by sales teams as a “cloud server.” In reality, what’s being offered is a cloud-hosted application that resides in their datacenter. It is not a server in the traditional sense, and it does not manage or support your local network. It simply runs the practice management software, which typically represents only about 10–12% of your total IT infrastructure.
My goal is to ensure the other 88–90%—your network, devices, and daily workflows—are running smoothly and securely. That’s where the true impact on your operations is felt, and that’s what this server is designed to support.